Life With A Pump
Saved by the Pump
Hi I’m Allan, aged 47, married with 2 young daughters and have been Type 1 since aged 19. In my job as an Aircraft Maintenance Engineer, safety of the aircraft fleet and everyone working or flying on them is the highest priority. For me that means Diabetic control must be maintained at all times, and on shift work, with a huge variation in work load & type, this takes a lot of achieving. On top of this there’s a whole pile of H&S bureaucracy ready to bite me if I don’t keep well controlled.
History
Luckily I have been OK for the last 28 years as I’ve not only managed to keep my job, but have also avoided any Diabetic complications. Most of the credit goes to the wide range of Health Professionals involved in Diabetes Management, as, without the Insulin, and associated equipment, test gear, R&D, plus, diagnosis, advice and support over the years, I would have reached my sell by date over a ¼ century ago! A small part of this may possibly be down to my choice not to smoke, and my Diabetic reaction to alcohol, which made drinking a non-starter. Oh OK, so I did drink for a couple of years prior to becoming Diabetic, but not enough to miss it when I had to give up!
My first syringe was a ‘Jules Verne’s’ looking, metal & glass instrument which was high maintenance and only used once a day. In case you think one injection a day would be ‘a cruise’, consider the planning required to align meals with the 4 hourly peaks the Insulins of that time were designed to produce, and whilst on shift work too! With only urine testing to rely on, the results were history even before doing the test. This meant every move had to be carefully thought through, like a never ending game of chess.
There were considerable improvements over the years such as disposable syringes, blood glucose testing, better Insulins including standardization to u100 strength. Some of these changes took a bit of a learning curve, however, all helped improve control significantly. Once the rate of innovation had slowed I settled into a ‘comfortable’ position where my Diabetes was reasonably well controlled.
There were considerable improvements over the years such as disposable syringes, blood glucose testing, better Insulins including standardization to u100 strength. Some of these changes took a bit of a learning curve, however, all helped improve control significantly. Once the rate of innovation had slowed I settled into a ‘comfortable’ position where my Diabetes was reasonably well controlled.
Setbacks
Then, 15 years ago I was knocked off my pushbike and suffered a head injury leaving me with badly degraded senses of taste, smell, and both long & short term memory problems. Without going into detail, this caused me very occasional missed or (worse still) double doses if insulin to be injected, for which I never managed to find a reliable method of prevention.
At the time I worked in the relative safety of the hangars where the work was of an overhaul nature, i.e. a steady pace, and involving lots of people. Everyone knew me and was aware of what to do in the event of a hypo. In this situation the risk of injury as a result of a hypo would be unlikely so the problems caused by poor memory were deemed tolerable. Recently, due to the recession in the aviation industry I had to transfer to operational aircraft work at the airport terminal. This meant working on several aircraft at a time spaced up to two miles apart, on 12hr shifts, with no set meal breaks, sometimes alone, and always to tight deadlines.
Just to make matters more interesting, I have been denied a permit to drive airside so getting about with tools & spares is done on foot, averaging nine rushed miles per day.
Saved
My response to this dramatic change was to run my BG deliberately higher than preferred during work hours in order to build in a ‘safety margin’ to avoid a hypo. This resulted in a significant rise in my HbA1c, which Dr Gallen spotted, and advised that this was unacceptable.
An Insulin pump was deemed to be the ideal answer and has proven itself beyond expectations over the last 8 months. Lots of people have their own reasons for preferring pump therapy but I think mine are a little different.
The pump history keeps a full record of all the Insulin taken so double doses are impossible. Missed doses can’t be prevented, but there’s no safety risk with this, and due to the frequency of blood tests would be picked up within a couple of hours anyway.
The theory
Injection therapy tended to be fixed dose and relied on regulating CHO intake and adjusting exercise to achieve acceptable BG levels. This was always at best, trial & error with any success being due to tremendous discipline. Pumping is a whole new step-change; you eat what you need (or want) to, or even skip a meal, and vary your bolus Insulin intake as required to keep the BG’s in limits. To make this method work, everything is quantified and tabulated. Your weight & lifestyle gives a specific CHO intake per day. From this a matching Insulin intake is calculated and split into basal & bolus doses. For the basal rate, you adjust to give a level BG under fasting idling conditions. This can be adjusted to a different rate every hour if needed so you can ‘iron out’ the dawn phenomenon and other such variables. For the bolus aspect there are several things to consider but initial settings are calculated for you, and you are given a set of figures to work to; Insulin ratio = how many grams of CHO to eat per unit of insulin, typically 10g:1u. Insulin sensitivity = how much your BG drops per unit of Insulin taken. Mine is 2.5per 1u for example and this is used to drop high BG’s quickly but safely. This seems strict but all this info and more is tabulated to help you make changes to pump settings and know beforehand with confidence what to expect. It’s so much safer than guesswork.
Injection therapy tended to be fixed dose and relied on regulating CHO intake and adjusting exercise to achieve acceptable BG levels. This was always at best, trial & error with any success being due to tremendous discipline. Pumping is a whole new step-change; you eat what you need (or want) to, or even skip a meal, and vary your bolus Insulin intake as required to keep the BG’s in limits. To make this method work, everything is quantified and tabulated. Your weight & lifestyle gives a specific CHO intake per day. From this a matching Insulin intake is calculated and split into basal & bolus doses. For the basal rate, you adjust to give a level BG under fasting idling conditions. This can be adjusted to a different rate every hour if needed so you can ‘iron out’ the dawn phenomenon and other such variables. For the bolus aspect there are several things to consider but initial settings are calculated for you, and you are given a set of figures to work to; Insulin ratio = how many grams of CHO to eat per unit of insulin, typically 10g:1u. Insulin sensitivity = how much your BG drops per unit of Insulin taken. Mine is 2.5per 1u for example and this is used to drop high BG’s quickly but safely. This seems strict but all this info and more is tabulated to help you make changes to pump settings and know beforehand with confidence what to expect. It’s so much safer than guesswork.
The tools
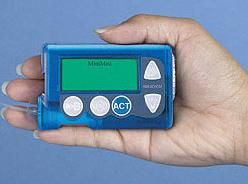
You’ll need to choose a make & model of pump, and if you’re on shift work, check the specs of all pumps on offer very carefully before choosing. This seems to be a big area of neglect for both pumps and BG meter/log software. I have found my BG meter log and associated PC software to be hard work when trying to make it ‘fit’ shift work. Good ‘olde fashioned parchment’ logging still seems to be easiest to work with, and if you have access to a scanner you’ll be able to e-mail your data to your Diabetic Nurse team just as well as if you were using the BG meter software. As for the pump, my own one makes a token gesture at catering for shiftwork….only for one function and even then, only if it fits into a 7 day pattern.
To complement the high precision of a pump a ‘Diet computer’ is a great tool to have. As well as CHO they hold several other nutritional values for over 400 different foods so all you need do is dial in a 3 digit code for what you are measuring and press the CHO button. The display reads directly in CHO, so you don’t even have to check what it weighs. It also has all the usual memory features of a typical calculator and retains data when switched off. You can shock yourself by recalling how much you’ve really eaten in a day!!! The one pictured is a Swiss instrument so the meat section is heavily biased towards Swiss/German love of sausage! There are ‘designer label’ British machines available which hold data for more of the branded foods sold in the UK, cereals for example. Of course, you can enter data manually and I only regularly use 20 or so of the 425 preprogrammed entries, plus about 5 that I’ve changed to my own values. And of course, if you are into cooking, it makes a very accurate set of weighing scales too with fluids displayable in ml, g, or oz, and weights in g or oz .
The other must have is a manual called Pumping Insulin. I tried a few books that my local library could get for me, and found them to be very lacking in technical data. This one is not available, even in the big UK bookshops, but can be obtained very easily and cheaply through the first online bookseller that comes to mind. Yes, the jungle one! (ISBN 1-884804-84-5).
The training courses given by pump dispensing hospitals do tell you what to do, but they simply don’t have time to go into why you need to do it. This book goes into enough detail to leave you well informed and able to diagnose problems with confidence, but not so much that you’ll be confused.
Once you’ve got over the novelty of pump operation, you’ll be hungry for details of how to fine-tune & troubleshoot Diabetic control on a pump, and this book is the best I’ve come across. Most of the figures for BG are given in UK and USA units, and the occasional entries that have mmol/L left off can be compared to one of the many useful charts a few pages fwd or back.
Supplies of pump consumables are direct from the manufacturers, as they are non-prescription items, with settlement of your account by direct payment by your PCT. You need to get this set up well in advance of attempting to place an order.
These two items are ‘must haves’ to go with a pump
Advantages/Disadvantages
For my own personal situation, the main advantage of a pump is the high level of safety with regard to hypo avoidance without sacrificing tight control. By using the metered bolus facility (square wave) a meal bolus can be given over a long period. For example, had I taken a normal bolus (or injection) for a meal based on an expected easy day, and the situation subsequently changed to become very busy, I would not be able to suck out what I now wish I had not injected! With a bolus over time, I have the option to suspend the delivery in order to prevent a hypo or remove the need to eat more CHO. In the event of a hypo occurring, suspending the pump helps slow or even reverse the onset. On taking glucose, no further complex CHO’s are required to prevent re-occurrence of a hypo.
Of course the other advantages are that you can’t forget to take your insulin with you, as it’s permanently attached, and for those who never liked taking injections, there are none. Once the pump is fine tuned to provide a near normal BG, it takes a lot of the hard work out of achieving good control.
There are a few disadvantages but once pumping becomes ‘the norm’ these disadvantages become unnoticeable to you.
The biggest one is that because Insulin supply is made to be as close as possible to ‘on demand’, there is no residual pool of insulin in you ( as an injection would provide) to damp out an unplanned glucose intake, or possible insulin delivery interruptions. The result is that the BG can soar to high levels very quickly if you eat too much or interrupt the pump delivery. On pump therapy, it’s normal to take about 8 BG tests per day which would catch this rise before it causes any serious problems, such as ketoacidosis. Some may see this level of testing as a disadvantage in itself, but it’s amazing how quickly this attitude reverses. When I was on injections, on a non-driving, non-working day I got away with as few as two tests per day, without any concern. Now I feel very insecure if I don’t know what my BG is doing.
The fact that the reservoirs are supplied empty is somewhat annoying. Filling them is a bit fiddly if using Insulin straight from the fridge as the bubbles stick firm! The adaptors and plungers all contribute to unnecessary environmentally unfriendly waste, and adaptor disposal requires costly biohazard waste handling. The sooner the pump producers supply pre-filled reservoirs the better it will be for all concerned.
Wearing the pump soon becomes normal, and is no worse than carrying a mobile phone, and won’t be anywhere near as annoying!
Reliability
Whilst I’ve only got 8 months experience, it’s usual that if something is going to go wrong, it will do so during the learning stage and/or when the equipment is relatively new. My pump has been totally reliable over this time with not even a spoiled or blocked insertion set. The insertion sets stick well for the full 3 days and the only time I’ve had one fall off is after a heavy morning gardening in hot sun where I was very hot & sweaty and moving around a lot. The set had done 2 ½ days, and under those conditions it was probably a good idea to change site early anyway. Swimming for long periods in the sea doesn’t seem to affect adhesion either. An altitude increase causes normally invisible bubbles to become big enough to upset BG control, so keep a watchful eye if you fly, ski mountain climb, etc.
Insurance
I found that some insurers won’t cover a pump, but the place to look is under home contents in the personal possessions section (which is usually an optional extra policy section). Due to the cost it will need to be recorded as a ‘specified item’, and as such, for some insurers, will not be covered by the automatic index linking. You may have to manually re-advise them of price increases. With this section activated cover is included away from home so you don’t need to go through all the pain of getting it insured under holiday insurance. On my policy, an item insured under personal possessions as a specified item carries a slightly higher excess than other contents items, but it’s still negligible when considering the cost of replacing one of these pumps.
Driving
On reporting this new treatment to DVLC medical dept, they don’t appear concerned that you can be driving whilst insulin is being administered automatically. It still only requires a 3 yearly renewal review, but it would be advisable to let DVLC know you’ve changed treatment.
Summary
Well, that’s probably enough info to give an overview of Pump therapy. Multiple injection therapy, using some of the pump therapy best practices described in the book would help improve control issues, but the best feature of the pump for me is the safety associated with delivery over time and delivery records.