Carbohydrates and Sports
Training and Competing with Type 1 Diabetes
Carbohydrates are the body's preferred energy source and are used by the muscles during exercise. It is recommended that you stick to your normal diabetic diet on rest days. On training days you may need to increase your carbohydrates, the quantity you need depends on how hard you train.
Carbohydrate Feeding and Exercise
It is recommended that your main meal 2-3 hours before exercise is carbohydrate based.
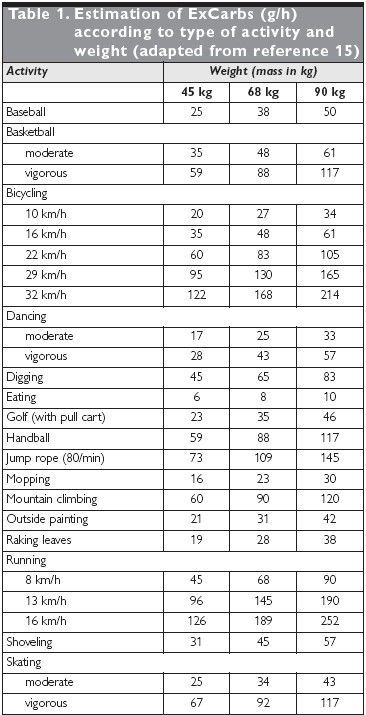
Calculating carbohydrate requirements
Immediately before exercise
With diabetes it is likely that you will require an increase in carbohydrates before exercise in order to maintain blood glucose
E.g. 2 - 3 digestives, 3 -5 jaffa cakes, 1 - 2 glasses of a glucose containing drink, a currant bun.
During exercise
Carbohydrate feeding aims to maintain adequate blood sugars.
The easiest way to ensure adequate blood glucose is to consume a sports drink throughout activity, this way you will also receive enough fluids. Other wise if there are intervals in your activity try jelly babies, jaffa cakes or glucose tablets.
Post exercise
Your muscles will be taking up more glucose from the blood to replenish their stores, especially during the first 2 hours. Check your blood sugars hourly after exercise. It is likely that carbohydrate based snacks will be required, particularly after prolonged exercise to prevent delayed hypoglycaemia.
Your muscles will be taking up more glucose from the blood to replenish their stores, especially during the first 2 hours. Check your blood sugars hourly after exercise. It is likely that carbohydrate based snacks will be required, particularly after prolonged exercise to prevent delayed hypoglycaemia.
During exercise there are three main possibilities
In well-controlled diabetes, blood glucose levels should remain fairly stable. Appropriate snacks are taken before and during exercise and insulin concentration is adjusted in advance of the exercise. This is what you should be aiming for.
In well-controlled diabetes, blood glucose levels should remain fairly stable. Appropriate snacks are taken before and during exercise and insulin concentration is adjusted in advance of the exercise. This is what you should be aiming for.
In poorly controlled diabetes where there is insufficient insulin or excessive carbohydrate is taken before or during exercise blood sugars rise leading to hyperglycaemia. Hypos are rarely experienced in this situation but you may become dehydrated.
If there is increased insulin (when exercising shortly after injecting insulin) or no extra snacks are taken before or during exercise blood sugars decrease. Blood sugars are taken up by the muscles leading to hypoglycaemia.
It may be necessary to either decrease insulin (discuss with your diabetes specialist nurse) and/or increase carbohydrate intake prior to or during exercise to avoid hypoglycaemia.
Recommendations
Try to AVOID exercising alone.
Try to AVOID exercising alone.
Educate your coach/trainer on how to recognise and treat hypoglycaemia.
Test your blood sugars more often, particularly before, during and hourly after exercise, this will help you understand your body's response.
If ketones are present with high blood sugars (>13 mmols/l), or if blood sugar levels are very high (>17 mmols/l) don’t exercise as this could lead to keto-acidosis.
If blood glucose is below 7mmols/l before exercise take additional CHO.
It is advisable not to exercise if blood glucose is below 4mmols/l.
Avoid exercising at the peak of your insulin.
Be prepared to either decrease insulin, increase pre/post exercise carbohydrate snack or both.
Always use the abdomen to inject insulin as insulin absorption is increased if injected into an active limb.
Always carry glucose - you may find a bum bag useful or take a sports drink.
Make sure you drink plenty of fluids during prolonged activity.
It will take time to understand the alterations that you need to make.
Things to consider when planning ahead
1. When does your insulin peak?
1. When does your insulin peak?
2. What type of exercise are you going to do and when?
3. When is your main meal and will it be carbohydrate based?
4. What is your pre exercise blood glucose?
5. What type of carbohydrate will you carry during exercise?
6. Will the temperature be very hot or cold?
7. Will you have plenty of fluids available?
8. What snacks will you have post exercise to avoid delayed hypoglycaemia.!