What are "Complications" of Diabetes?
Complications
of diabetes are the changes in the body caused by high glucose levels.
The can be acute or chronic. The acute complications included the most
severe complications of coma and death. High levels of blood sugar lead
to thirst, the passage of large quantities of urine and dehydration. In
the extreme form, blood glucose levels rise and loss consciousness
ensures, and ultimately, without treatment death occurs. Fortunately
this is very rare. A further and much more common cause of coma is due
to low blood glucose (hypoglycaemia), which is the result of either
insulin or tablets treatment.
The chronic complications of diabetes develop over many years, and are the result of high blood glucose levels. Even if the symptoms of diabetes are relieved by treatment, it may not provide adequate blood glucose control. As a result of long-term high blood glucose values in apparently well people, further secondary damage to virtually every tissue in the body can occur. The eyes, kidneys, blood vessels and nerves are prone to damage. The thickening of the small blood vessels (capillaries), leads to reduce transfer of oxygen and other nutrients to the tissues. This process is known as micro-angiopathy.
The chronic complications of diabetes develop over many years, and are the result of high blood glucose levels. Even if the symptoms of diabetes are relieved by treatment, it may not provide adequate blood glucose control. As a result of long-term high blood glucose values in apparently well people, further secondary damage to virtually every tissue in the body can occur. The eyes, kidneys, blood vessels and nerves are prone to damage. The thickening of the small blood vessels (capillaries), leads to reduce transfer of oxygen and other nutrients to the tissues. This process is known as micro-angiopathy.
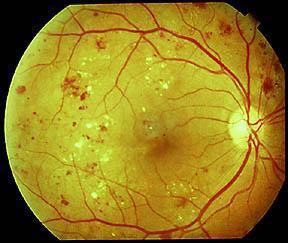
Diabetes and the Eyes
The
most feared diabetic complication is blindness. Fortunately, this is
now very rare in developed countries, but still is a common cause of
blindness elsewhere in the world. Diabetes can damage the light
sensitive part at the back of the eye, the retina. At your clinic
visit, you need to have a thorough retinal examination either by
retinal photography, or by ophthalmoscope having had your pupils
dilated with eye drops first. Ask your doctor what changes if any are
present and how they should be managed. The terminology for these
changes is graded from the early background retinopathy, to the more
severe maculopathy, and most seriously the sight threatening
proliferative retinopathy. Cataract is when the lens at the
front of the eye becomes opaque. High glucose levels cause the changes
in the retina, which leads to blood vessel closure and increased blood
pressure within the retina. There is leakage of blood and blood
products from these small blood vessels, the formation weaknesses of
blood vessels (micro aneurisms), and small haemorrhages within the
retina. This initial phase is classified as background
retinopathy. When this occurs in the most sensitive part of the retina,
the macula, loss of visual acuity follows and may progress to
blindness. This process, (maculopathy), is most frequently seen in
Type 2 diabetes patients who have raised blood pressure, and is
aggravated by smoking. As the damage continues, new thin walled and
fragile blood vessels are formed (proliferative retinopathy). Haemorrhage
from these vessels can cause acute loss of sight, which may clear. Organisation of the haemorrhage causes fibrosis within the retina,
which can cause retinal detachment and blindness. Diabetic retinopathy
can be avoided or the progression can be slowed by having the best
blood glucose control possible, by the use of blood pressure
loweringdrugs, particularly the ACE inhibitors drugs, and with the
early use of laser treatment.
Kidney Disease
High
level of glucose over many years damages the kidneys. The filtration
unit, the glomerulus, becomes thickened and scarred. Unfortunately,
there are no symptoms until it is too late. The first clinical sign of
this process is the passage of small quantities of protein in the urine
(microalbuminuria). This needs to be checked at your clinic visit. If
the damage continues, it will lead to kidney failure, which has to be
treated by a kidney transplant or dialysis. Again it can be avoided or
having the best blood glucose control possible, by the use of blood
pressure lowering drugs, particularly the ACE inhibitors drugs, can
slow progression.
Nerve Damage and Feet
Damage
to the nerves in diabetes has many causes. Nerves and their supporting
tissues can be damaged by loss of blood supply due to, by high levels
of glucose, and by alteration in the composition of the nerve structure
induced by hyperglycaemia. Loss of nervous function leads to loss of
sensation from the limbs and joints, muscle function and control of the
internal organs such as the heart, stomach and bowels, and of the
bladder and reproductive system. In the foot, there is increased risk
of skin ulceration and infection, unsuspected fractures of the small
bones causing deformity and eventually amputation.
Arterial Disease
There
are very high rates of angina or heart attacks (myocardial ischaemia
and infarction), stroke, and peripheral vascular disease in diabetes.
Fatty deposits called atheroma can narrow arteries all over the body.
The process of narrowing of arteries can be seen in non-diabetics, is
accelerated in diabetes. The effect depends on which part of the body
is supplied by the narrow artery. It is therefore vital that risk
factors for these changes are controlled. Blood pressure, blood
cholesterol and blood glucose all need to be managed appropriately, and
medication to alter the stickiness of the blood cells (platelets),
usually aspirin used.