High-Intensity Exercise and Hypoglycaemia
High-intensity
exercise may be defined as activities above the ‘lactate threshold’.
This occurs when there is an exponential increase in lactate production
caused by a greater reliance on anaerobic metabolism, occurring at
approximately 60-70% of VO2max or 85-90% maximal heart rate. This
threshold coincides with dramatic elevation in catecholamines that
increase hepatic glucose release, FFA, and ketone levels, and impair
glucose utilization by skeletal muscle (Fig. 1C). Even
those individuals treated with intensive insulin therapy may have
increases in blood glucose levels during and after high-intensity
exercise, probably due to a failure in insulin release to offset the
increases in counterregulatory hormones. This rise in glucose
concentration is usually transient and tends to last only as long as
there are elevations in counterregulatory hormones (i.e., 30-60 min).
Although
some individuals can easily correct the elevations with an insulin
bolus, particularly if they take rapid acting insulin analogs, others
may be reluctant to take additional insulin after exercise, because
there will be greater risk of late-onset postexercise hypoglycemia.
Competition Stress, Heat Stress and Hyperglycaemia
The
psychological stress of competition is frequently associated with
increases in blood glucose levels even though the pre-exercise glucose
concentrations may be normal. Those pursuing vigorous aerobic exercise
may find that on regular training or practice days they become
hypoglycemic, but on the day of competition they develop hyperglycemia.
Although empiric data do not exist for children with T1DM, excessive
increases in glucose counterregulatory hormones probably occur just
before exercise when anticipatory stress is high. It is also probable
that the stress during competition can further increase blood glucose
levels. Individuals may find that play or sporting activities in warm
and humid environments also elevates blood glucose levels, probably
because of excessive increases in circulating plasma catecholamines,
glucagon, cortisol, and growth hormone (Fig. 1D).
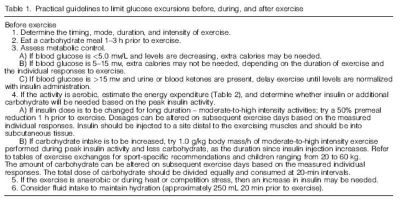
Practical considerations for the clinical management of type 1 diabetes in athletic youth
The
major challenge for active youth with T1DM is to balance food, insulin,
and exercise to limit blood glucose excursions. Some of the factors
affecting blood glucose levels during exercise are circulating plasma
insulin levels, the intensity and duration of the exercise, the type of
exercise performed (aerobic vs. anaerobic), and the prevailing
concentrations of the glucose counterregulatory hormones. To a lesser
extent, age, gender, level of metabolic control, and the level of
aerobic fitness also contribute. Although the glycemic response varies
greatly between children, blood glucose changes during exercise have
some degree of reproducibility, as long as the exercise conditions and
pre-exercise insulin and diet are consistent. Whereas no precise
guidelines exist to limit fluctuations in glucose levels during
exercise, some general strategies do exist (Table 1).
Importantly,
a well-organized plan should be developed and conveyed to the child’s
coaches, teachers, friends, guardians, and siblings. Children and
adolescents should delay participation in physical activity if blood
glucose levels are below 60 mg/dL (<3.5 mmol/ L) or above 270 mg/dL
(15.0 mmol/L) with detectable urine or blood ketones. Practical
recommendations to help prevent hypo- and hyperglycemia are provided
below and are summarised in Table 1.